Displaying items by tag: medical
Diagnosing the Attempted NARAL Attack
by Susan Dammann, RN, LAS, Medical Specialist
As we examine the symptoms exposed in the recent report unveiling the state chapter of NARAL Pro-Choice America colluding with Maryland government officials, a diagnosis becomes quite clear. This legal effort to shut down a local pro-life pregnancy care center, along with a seven-part plan developed by NARAL to shut down pregnancy help organizations across the country, reveal an infection with the intention to spread.
Miriam Webster defines diagnosis as"the act of identifying a disease, illness, or problem by examining someone or something."
First, there is definitely a primary source of infection, still seemingly localized, and the infection's focal point is limited to a small segment of the population. In 2010 when "Montgomery County passed an ordinance requiring Centro Tepeyac Silver Spring Women's Center and other pro-life pregnancy care clinics to post signs stating that they did not have doctors on staff," the outbreak was cured by three court decisions against the ordinance.
"Judge Deborah Chasanow, a Clinton appointee, noted that the people who accused the centers of spreading 'misinformation' were 'universally volunteers from a pro-choice organization sent to investigate practices' at the centers."
[Read Heartbeat President Peggy Hartshorn’s Op-Ed at LifeSiteNews.com here.]
When we learn of such outbreaks it is common to wonder if this will erupt into an epidemic or pandemic. Then we wonder how we can immunize ourselves from being attacked by the same germs.
The very best way to inoculate ourselves is to do just as they have already given us credit for doing!
The County responded to NARAL with the following statement: "I doubt my colleagues or the County Attorney will be interested in pursuing a truth-in-advertising statute...[these centers] are clearly very artful at devising strategies to avoid violating the law." Strategies to avoid violating the law simply put, means we obey the law and they recognize it. Your best immunization plan is to keep up your mission and the excellence with which you always work. You can always take your organization's vital signs by checking up on our Commitment of Care and Competence.
It would be a misdiagnosis if we thought we could treat these germs by pregnancy help organizations hiring doctors and nurses, putting in state of the art equipment and following all the best practices so that they will approve of us and stop the attacks. We have done just that and they are still manipulating women with lies and misleading information.
True choice and excellent healthcare for women are not their goal. The accurate diagnosis is that the abortion industry has a goal of permanently eliminating pregnancy centers because we are undermining their bottom line of profit.
Keep in mind that we do not live in a sterile environment and that germs abound. We can expect that by making inroads to bring health and wholeness into our world, there may be attacks. This is to be expected, but not feared. God even tells us in His Word that we may suffer for the sake of righteousness, but we are blessed.
"But even if you should suffer for the sake of righteousness, you are blessed. And do not fear their intimidation, and do not be troubled." 1 Peter 3:14 NASB
What Insurance Should We Carry?
 by Paula Burns, CIC, CRM, Insurance One Agency, LLC
by Paula Burns, CIC, CRM, Insurance One Agency, LLC
Knowing what kind of insurance your Pregnancy Help Organization may need can be difficult. Beyond the general questions of what should be covered, each state has specific mandates or benefits about certain types of insurance. We sat down with Paula Burns from Insurance One Agency to find out what they would recommend.
Pregnancy Help Organizations (PHOs) are on the front line in the battle to save human lives and souls. They are the ultimate picture of the “Great Commission” coming to fruition and want every ministry dollar to go into the purpose and mission of the ministry, not into liability litigation. As a result, there are many questions frequently proposed regarding insurance for the centers and the wide scope of risk associated with them. This article includes a brief overview of insurance coverage a PHO should carry in their insurance coverage portfolio and addresses some of the most frequently asked questions.
Q: What is a general overview of insurance coverage a Pregnancy Help Organization (PHO) should carry?
A: Pregnancy Help Organizations should in general have the following in their insurance coverage portfolio:
- Package Policy which includes:
- Property coverage- covers contents, outdoor signs, computers & equipment, buildings, or if rented location can include rental space betterments and improvements. Business Income/Extra Expense are normally included to cover loss of income and extra expense to run the PHO should the organization be shut down for a period of time due to a covered claim, and resulting expenses if they have to relocate.
- General liability coverage- premises liability, personal injury, advertising injury, and general liability for your day to day operations of running the PHO that are not professional in the scope of duties. Volunteers normally are included in this coverage as insured’s. (Very important that volunteers are included in the definition of “Who is an Insured” on the PHC General Liability coverage portion of the policy.)
- Medical Payments –This coverage is very important in that it is a “no fault” coverage that will protect the PHC from minor slip and fall claims/incidents that result from NO negligence on behalf of the PHC.
- Crime- covers employee theft, forgery, theft or burglary of money and securities.
- Inland Marine – Specialty equipment scheduled here. Sonograms are one example of property commonly scheduled on an inland marine form. Mobile sonograms would be part of an inland marine form, but stationary sonograms are normally included in contents coverage.
- Sexual Misconduct Coverage – Be sure this is included in the coverage to protect not only the Sonographers, but the Client Advocates as well. This coverage is important to protect staff and volunteers from false allegations. Insurance One has many resources to assist with training to reduce this risk.
- Professional Liability Coverage- Many policies will cover the Professional Liability exposure for your Medical Director, Nurse, Sonographer, Executive Director,& Client Advocates. Be sure that this coverage includes vicarious liability. This topic is covered later in the article in further detail. Every insurer’s forms are different regarding Professional Liability; be sure to ask if the above Professionals are covered.
- Directors & Officers Including Employment Practices Coverage:
- Directors & Officers coverage will extend to the individual Directors and Officers of the organization and protect them from errors or omissions in their governance of the organization. This is a very important portion of the coverage portfolio. There is a general misconception that the Directors and Officers are covered under the General Liability policy, but they are actually excluded on that policy, therefore leaving a huge exposure for the organization and Directors individually.
- Employment Practices Coverage* in general will extend to cover the following claims of:
- Wrongful termination / breach of employment contract
- Wrongful failure to promote
- Violation of employment discrimination laws (including harassment)
- Sexual harassment
- Employment related retaliation/ humiliation
- Employment Related wrongful discipline
- Negligent employee evaluation
- Wrongful demotion/ Negligent reassignment
*Note: The insurance carriers are seeing a large number of claims resulting from Employment Practices. It is key to be sure your PHO is carrying this coverage.
- Automobile Coverage
- Even if the PHO does not own an auto they have two additional exposures:
- Covers autos owned by the PHO
- Hired Auto – when someone from the organization rents a vehicle this coverage will extend and cover the liability portion of the coverage for the car rental. This does not include damage to the rental car itself so it is always a best practice to purchase the Physical Damage coverage (also called the LDW – Loss Damage Waiver) from the rental car company directly.
- Non-Owned Auto* – extends to cover the organization’s defense costs should a staff member or volunteer drive their own personal vehicle on behalf of the PHO.
- Even if the PHO does not own an auto they have two additional exposures:
*Note the employee or volunteer’s vehicle insurance is ALWAYS primary if they are driving their own vehicle on PHO business.
- Umbrella Coverage
- Additional layer of coverage normally carried in increments of $1,000,000 that extends additional coverage for liability driven claims, normally for the following:
- General Liability
- Professional Liability
- Employer’s Liability
- Automobile Liability
- Sometimes this is also extended to include Sexual Misconduct Liability
- Additional layer of coverage normally carried in increments of $1,000,000 that extends additional coverage for liability driven claims, normally for the following:
- Worker’s Compensation Coverage
- Wikipedia’s definition is excellent and defines this coverage as follows; “Workers' compensation as a form of insurance providing wage replacement and medical benefits to employees injured in the course of employment in exchange for mandatory relinquishment of the employee's right to sue his or her employer for the tort of negligence.”
- Every state’s laws vary regarding Worker’s Compensation. Some will mandate that Worker’s Compensation is carried by every employer with a certain number of employees. Texas, for example, does not mandate that employers have to carry Worker’s Compensation, however; the employer loses certain common law defenses if they do not subscribe to Worker’s Compensation. Be sure you understand the laws in your state and how it applies to your PHO operations.
Q: Should a PHO carry Worker’s Compensation Coverage? Will a PHO staff member’s personal health insurance coverage cover them if they are injured on the job?
A: As discussed in the section above, state law is going to mandate whether a PHO is required to carry Worker’s Compensation. If the state is not mandating that the PHO carry this coverage there are multiple considerations:
- First of all, an individual’s personal health insurance normally excludes work related injuries. That personal health insurance will cover employees injured on the job is a huge misconception with many organizations. They think because the individuals they have on staff carry health insurance that they do not need to carry Worker’s Compensation coverage. Nothing could be farther from the truth.
- Another common misconception is that this coverage is expensive. In fact, Worker’s Compensation is one of the cheapest coverages you can purchase in your entire coverage portfolio and it is a huge benefit to the employees. PHOs do not want to put their employees in the position of not having coverage should they be injured on the job. This could result in litigation against the PHO if there are medical bills that cannot be paid, loss of wages, and potentially even an injury that could result in the inability to continue working.
- Many states will give additional defenses if the organization subscribes to Worker’s Compensation. In Texas, for example, the organization gains the common law defense of assumed risk. Assumed risk is a hazard assumed to be part of the job duty. For example, if the organization hires an employee to take care of the yard maintenance, it is assumed that they might get something in their eye from the mowing of the lawn or some other type of hazard related to yard work, etc. The employee then could not sue the employer because they had this type of injury.
Be sure to check your state laws regarding Worker’s Compensation!
Q: Will a physician’s insurance automatically cover the pregnancy center?
A: No, the physician’s insurance may not extend on a volunteer basis. Professional liability policies are not standardized and therefore, literally every insurance carrier’s forms are different. Please ask this question up front and find out if the physician’s coverage will extend. Even if their coverage extends it normally is only going to cover them individually, it does not normally extend to cover the PHO and release them from claims of vicarious liability. The PHO needs to do some due diligence to reduce their risk regarding this exposure and some recommendations are as follows:
- Always make sure that you have on file a copy of the doctor’s license and that it is up to date and current.
- Keep a copy of the doctor’s Certificate of Insurance on file and update it on an annual basis at renewal.
- Verify if their coverage extends on a volunteer basis.
- It is important that the PHO consult with an insurance agent who understands this exposure and can design a coverage portfolio to pick up the doctor while they are acting in the capacity of Medical Director for the PHO. Some coverage forms will extend to the doctor if they are formally named the Medical Director. This is literally the coverage trigger in the policy. Your insurance advisor can walk you through this and be sure that your coverage gaps are filled.
- Be sure that your coverage includes vicarious liability. This is otherwise known as “guilty by association.” Be sure when you are referring clients to doctors or counselors that you give them a list as this will reduce your risk greatly. A claims example: The PHO refers a client to a specific doctor and there is a misdiagnosis resulting in some type of claim/loss. The PHO can be vicariously liable for this claim.
- The best case scenario is for the doctor’s coverage to extend on a volunteer basis and also include them in the PHOs coverage as well so all gaps are filled in the event of a claim.
In conclusion, the PHOs are operating in one of the most litigious environments to date and need to understand how to take a proactive stance towards risk. One component of a good risk management plan is insurance, however, insurance should never be substituted for risk management. It is important that every PHC have a good comprehensive training program in place for their staff and volunteers. This is the first line of defense against liability claims and is for their protection as well as the PHO.
Matthew 28:19-20 “Therefore go and make disciples of all nations, baptizing them in the name of the Father and of the Son and of the Holy Spirit, 20 and teaching them to obey everything I have commanded you. And surely I am with you always, to the very end of the age.”
 Paula Burns specializes in insuring larger churches and non-profit organizations and has been in the insurance industry for 29 years. She has earned the designations of Certified Insurance Counselor (CIC) and Certified Risk Manager (CRM). Her career began in property and casualty claims laying a foundation for Paula to be an advocate for clients when they need her the most, during a claim or crisis.
Paula Burns specializes in insuring larger churches and non-profit organizations and has been in the insurance industry for 29 years. She has earned the designations of Certified Insurance Counselor (CIC) and Certified Risk Manager (CRM). Her career began in property and casualty claims laying a foundation for Paula to be an advocate for clients when they need her the most, during a claim or crisis.
Paula is a faculty member of The National Alliance and teaches classes to other insurance professionals, risk managers, and non-profit organizations regarding risk management. When she is not teaching, or at the agency, you can find her on her horse farm close to Whitney, TX with her husband of 23 years. She and her husband Gary have two children, Brandon and Lindsey. She joined Insurance One Agency in 2010 because they have a heart to serve those who serve.
Insurance One has a national program that includes state of the art coverage designed specifically for Pregnancy Help Centers and many Heartbeat International and Care Net affiliates use this coverage. They understand the risks associated with insuring PHC's and partner with centers from all over the nation to protect their ministries. You can reach Insurance One Agency by clicking here.
Resources for Your Medical Director!
Our Medical Directors are a vital part of our Medical Clinics, and provide critical services for us often at their own expense and time. Here are some resources you can pass on to them to let them know how much we all appreciate them and their service to the clinics.
Physicians need 30-50 hours of AMA Category 1 CME to meet the AIUM requirements. Is your Medical Director looking for opportunities to sharpen his/her skills in reading Limited OB Ultrasounds?
American Institute for Ultrasound Medicine: www.aium.org
"Not to be missed is the 38th Annual Advanced Ultrasound Ob/GYN Seminar" http://www.aium.org/soundWaves/article.aspx?aId=865&iId=20150107
Learn From the Experts at the 38th Annual Advanced Ultrasound Seminar: Ob/Gyn
Come to Lake Buena Vista, Florida, this February if you want to expand your obstetric and gynecologic ultrasound knowledge with renowned experts in the field. View the program and register. Join Codirectors Lennard D. Greenbaum, MD, and Frederick W. Kremkau, PhD, along with ultrasound luminaries Alfred Z. Abuhamad, MD, Beryl R. Benacerraf, MD, Joshua A. Copel, MD, Steven R. Goldstein, MD, John C. Hobbins, MD, and Lawrence D. Platt, MD.
This seminar, hosted by the AIUM in collaboration with Orlando Health and the Wake Forest School of Medicine, will be held February 19-21, 2015, at Disney's Yacht and Beach Club Resorts in Lake Buena Vista, Florida. The seminar is filling quickly! Register today and earn up to 13.5 AMA PRA Category 1 Credits.
Do you have a physician who would like to serve your center as a Medical Director but is not trained to read OB scans? Please read through all the options available for them and pass the information along to them.
Below are some great options you can offer to them as resources for both initial training and refresher courses. While Heartbeat does not have any direct knowledge of the courses, these resources were recommended by an RDMS ultrasound trainer who serves in the pregnancy center ministry, and we are passing on the information for the physician to investigate and choose the course best suited for their needs.
Gulfcoast Ultrasound Institute: www.gcus.com
Thomas Jefferson University: http://www.jefferson.edu/university/jmc/departments/radiology/education/cme/ultrasound_courses.html
Wake Forest: http://www.wakeultrasoundeducation.com/courses-and-seminars/obstetrical-ultrasound/
IAME: https://iame.com/conferences/obgyn_ultrasound/
Another Great Resource From the AIUM:
Everything You Want to Know About First-Trimester Obstetric Ultrasound is a great learning tool for which physicians can earn up to 6.0 CME credits.
"After viewing this program, participants should be able to describe the sonographic signs of normal and abnormal gestations and define the role of ultrasound in the early diagnosis of fetal anomalies. The learner attributes are patient care, medical knowledge, and practice-based learning and improvement."
This DVD comes with 5 CME test and evaluation forms that allow you and up to 4 colleagues to earn credits at no extra charge. Need more than 5 tests? Purchase additional sets of 5 tests/evaluations for only $160.00.
New FDA Consumer Update Urges Women to Obtain Medical Sonograms with Trained Operators
By Susan Dammann RN
The FDA has issued a warning. While the FDA's main focus in the warning is to advise pregnant women to avoid commercial sonogram services for nonmedical purposes that could pose a danger to the developing fetus, emphasizing that these are prescription medical devices, are to be used only by trained health care professional and only with a prescription, included within the warning are guidelines/recommendations which we in the pregnancy help medical clinics should be aware of.
Below are three excerpts from the 12/16/14 FDA Consumer Update which may pertain to the use of ultrasound imaging in the PMC, and a question for you to consider.
"Fetal ultrasound imaging provides real-time images of the fetus. Doppler fetal ultrasound heartbeat monitors are hand-held ultrasound devices that let you listen to the heartbeat of the fetus. Both are prescription devices designed to be used by trained health care professionals. They are not intended for over-the-counter (OTC) sale or use, and the FDA strongly discourages their use for creating fetal keepsake images and videos."
Question: Are the sonograms in your center being performed by trained health care professionals?
"The long-term effects of tissue heating and cavitation are not known. Therefore, ultrasound scans should be done only when there is a medical need, based on a prescription, and performed by appropriately-trained operators."
Question: Are the sonograms performed in your center based on a prescription for a medical need?
"Similar concerns surround the OTC sale and use of Doppler ultrasound heartbeat monitors. These devices, which are used for listening to the heartbeat of a fetus, are legally marketed as "prescription devices," and should only be used by, or under the supervision of, a health care professional."
Question: If your center uses Doppler, is it being used under the supervision of a health care professional?
As you consider the above FDA recommendations in relation to the ultrasound services performed in your PMC keep in mind also that one of the points in the Commitment of Care and Competence to which all Heartbeat Affiliates sign in agreement is:
Medical services are provided in accordance with all applicable laws, and in accordance with pertinent medical standards, under the supervision and direction of a licensed physician.
To read the full FDA Consumer Update click here.
Ultrasound Safety – Revisited
by Kevin T. Rooker, RT(R), RDMS, RVT, Sonography Consultants
Is ultrasound safe? Will it hurt my baby? These are questions we sometimes hear from our clients. We need to be able to answer those questions with confidence for several reasons. First, because our patients deserve an honest answer, and second because we never know who is listening. We know that there are some that think you should not be performing limited OB ultrasound and will always be looking for reasons to justify their position. Let's not give them that opportunity on the issue of ultrasound safety. Unfortunately, we, the medical community, have not done as well as we can at educating ourselves on the safety of ultrasound1.
Ultrasound is a wave of mechanical energy that penetrates human tissue as an oscillating (alternating) wave of high and low pressure. As it does so, there are two potential types of biological effects; Mechanical and Thermal. In 1993, the FDA allowed ultrasound manufacturers to significantly increase the amount of ultrasound energy created in diagnostic ultrasound systems, as long as they displayed the MI (Mechanical Index) and TI (Thermal Index) on the screen for the operator (and our clients) to see. The premise being that if we know what the MI and TI are, what their limits are, and most importantly how to lower them, then we are being as safe as we possibly can.
The Mechanical Index is a safety metric which lets the operator know how much energy is being transmitted into the patient during a sonography examination. Remember that sound is created by pressure waves, so mechanical energy is transmitted into any object which receives sound. Sound waves can be quite powerful. For example, think of the thump on your chest when sitting next to a teenager's car with the high dollar stereo system. It is defined as the peak negative pressure (PNP) of the ultrasound wave (point of maximal rarefaction). In easier terms; think pressure change divided by time. Lots of pressure change over short periods of time can be damaging. The FDA has established a maximum MI of 1.9 for diagnostic imaging. Any machine capable of generating MI greater than 1.0 must display the MI onscreen. The FDA MI limit for obstetric sonography is 1.0.
The Thermal Index is another safety metric which lets the operator know the potential of creating heat (hyperthermia) with the ultrasound beam. Many assumptions are made in this calculation, and it is often thought that the heating potential is underestimated. So keep in mind that the TI formulation was not intended to, and cannot provide an accurate measure of temperature rise within a specific patient. Instead it was designed to provide the operator with a relative measure of risk for a particular imaging mode. A Thermal Index of one (TI 1) indicates conditions under which the rise in temperature would be likely to be 1°C. The thermal index is different for different types of tissue, and can be displayed on your system accordingly: soft tissue (TIs), bone (TIb) and cranium (TIc). In the first trimester, when using Doppler to hear and demonstrate the fetal heart, the TIs setting us used. The limit for TI varies with time, please reference the chart below from the British Medical Ultrasound Society, the entire document may be found here.
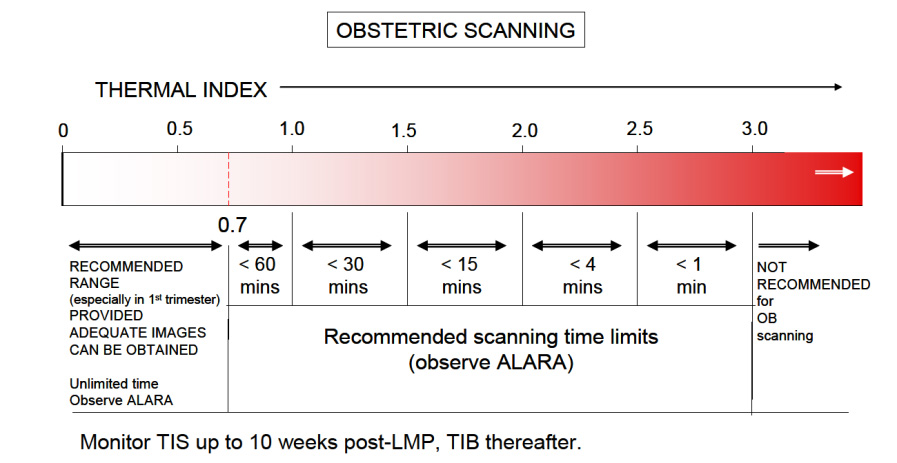
Enough about what the MI and TI are, how do we as operators keep them at safe levels? There are two basic concerns to remember.
First is the AIUM ALARA policy2; which is an acronym for As Low As Reasonably Achievable. Simply translated, it means to keep the output power settings as low as possible, that still allows for adequate images. Most ultrasound systems can operate with output power settings at about 50% and still produce quite satisfactory OB images. Have your system presets adjusted so that when you are performing OB sonography both (abdominally and transvaginally), the output power settings are set low. You can always increase them if clinically necessary. And keep in mind that you can increase the gain to make your image brighter, as gain is just how well the system is "listening", it has no effect on the TI.
The second concern is time. Keep the overall examination as short as is reasonable. If using Doppler to allow Mom to hear her baby's heartbeat, depending upon your ceter's policy, keep the Doppler exposure to about 5-10 seconds. Know where to find the MI and TI displays on your system. If you don't know, consult your operator's manual or contact the manufacturer of your ultrasound system for more information.
Diagnostic ultrasound in obstetrics has been around for the better part of 40 years. To date, no one has been able to prove (and many have tried) that diagnostic ultrasound, when used prudently (MI,<1.0 and TI<0.7), has had any adverse effects developing fetuses; and this includes the limited use of Doppler in the first trimester "Thus far, there have been no significant thermal effects documented in humans and at this time the possibility of having all the factors present to is highly unlikely 3." However, it has been shown that aborting a living fetus is fatal, every time.
References
1. Ultrasound Is Safe . . . Right? Resident and Maternal-Fetal Medicine Fellow Knowledge
Regarding Obstetric Ultrasound Safety. J Ultrasound Med 2011; 30:21–27
Sheiner E, Abramowicz JS. Clinical end users worldwide show poor knowledge regarding safety issues of ultrasound during pregnancy. J Ultrasound Med. 2008;27(4):499-501
2. As Low As Reasonably Achievable (ALARA) Principle Approved 4/2/2014 aium.org/officialStatements/39
3. FDA Recommendations for the Safe Use of Ultrasound in Obstetrics CNE article authored by Sherri A. Longo, M.D. Assistant Professor in the Department of Obstetrics and Gynecology, Division of Maternal-Fetal Medicine, Tulane University School of Medicine in New Orleans, Louisiana; e-edcredits.com/nursingcredits/article.asp?testID=29
Fuss about Practice Fusion?
By Jor-El Godsey, Vice President
If you don't know the difference between EHR and EMR and PHR, HIPAA and HI-TECH, EPM and PMS , PRC and PMC, then stop reading.
If you do, or think you do, you're probably knee-deep in medical clinic regulations and/or clinic practices.
Pregnancy help medical clinics have been growing in number and complexity for the last twenty years. Originally focused on ultrasound services, many life-affirming, medically savvy centers are expanding medical services to include STI testing/treatment, pre-natal care, and more.
Good business systems, important for all pregnancy help organizations, has been a dynamic question for medically focused affiliates with the changing nature of health care regulations.
Life-affirming friends like eKyros and WayCool that specialize in database solutions for pregnancy help organizations have been answering that question with increased security, encrypted records and other HIPAA-necessary implementations. However, some in our community have either opted for, or promoted other software.
One of those is Practice Fusion. And, yes, there has been a fuss about Practice Fusion.
Practice Fusion is presented as being "free" (always attractive to non-profits) and, despite its relative newness (launched in 2007), has been quickly accepted by doctors office across the U.S. There are, however, some troubling findings that ought to give life-affirming pregnancy help organizations pause.
First, is anything really "free"? The article, "What Makes Free EHRs Expensive in the Long Run?" rightly notes, "...hidden expenses, heightened risk and unforeseen liabilities can cost you just as much as any web-based EHR..." So always beware of any Open Source product being offered for FREE.
Second, venture capitalists have invested nearly $200 million in this product. How will they realize their return on investment? It's always good to look a little closer to understand how a free product is able to remain current, supported and adaptable for future innovation. An article from Business Week notes the following:
The company makes money by charging more than 70,000 pharmacies, 300 diagnostics labs, and 21 imaging centers for access to its captive community of medical pros. For example, labs pay for the convenience of transmitting test results rather than faxing them, while drugmakers pay to deliver targeted ads to doctors. For an additional fee, companies can use a Practice Fusion tool to sift through its trove of more than 80 million patient records to identify patterns, such why doctors might be choosing one drug over another. The data is stripped of any information that would reveal the identity of the patients. The company is also working with insurer Aetna (AET) to identify at-risk patients to head off costly trips to the emergency room.
A pregnancy help organization using Practice Fusion apparently becomes part of the "captive community" targeted by those profiting from offering this "free" product.
Third, Practice Fusion's own practices have created significant compliance and confidentiality questions. Some industry watchers have noted, that "[a]ccording to experts, it may have violated the grand poobah of medical privacy laws — HIPAA — potentially getting both the doctors and Practice Fusion — as a "business associate" — into trouble. Additionally, the Federal Trade Commission may see what the start-up did as a deceptive business practice."
Along with these three specific points about Practice Fusion (or free EHRs in general), there comes a much more basic question:
Is there value in working within our specialized world of life-affirming pregnancy help to sharpen a good tool for all of us to use?
We think so, and we encourage you to think carefully when considering such important business tools.
24 Hour Turn-Around on Ultrasound Scans?
Making Sense of AIUM Guidelines
Connie Ambrecht RDMS, Executive Director Equip Leaders Now/Sonography Now
Beverly Anderson, J.D., CEO Dove Medical
Susan Dammann RN LASm Medical Specialist
The Issue
In April 2014, the American Institute of Ultrasound in Medicine (AIUM) sent an email to its members stating it had "Updated Guidelines and Official Statements." Included in the list was the guideline titled "Documentation of an Ultrasound Examination."
First, it is valuable to revisit who AIUM is, as well as its role in ultrasound imaging. In its own words, "the AIUM is an association dedicated to advancing the safe and effective use of ultrasound in medicine through professional and public education, research, development of guidelines, and accreditation."
In the first section of the guidelines, AIUM outlines what it considers high-quality patient care. The guidelines state a permanent record should always be kept of the images, and an interpretation should be provided for patient records. All medical professionals involved should be able to communicate well and work as a team to provide what is expected: quality patient care.
The next section lists what should be included in the official report. In some clinical settings, the interpretation of the images is transcribed and a separate report page is generated for the patients chart. In the PMC setting it is common that a signature is obtained on the ultrasound report page and serves as the final report.
Section three discusses the final report from the interpreting physician or medical director of the clinic. According to this April 2014 update, the final report should be generated in 24 hours. I know you are thinking or asking... "How can we do that?!"
We restate the following from the AIUM guideline: Practice guidelines of the AIUM are intended to provide the medical ultrasound community with guidelines for the performance and recording of high-quality ultrasound examinations. The guidelines reflect what the AIUM considers the minimum criteria for a complete examination in each area but are not intended to establish a legal standard of care.
This AIUM Guideline is NOT a legal requirement. It is a national practice standard.
We at Sonography Now live in the service trenches with you as we train on-site. We understand that getting interpretations in a timely fashion versus every 24 hours can seem unnecessary. Taking one step at a time can ease such a transition. If you want to make changes to accommodate a faster interpretation time, it doesn't need to change immediately.
Building a plan of action can remedy the feeling of urgency. Some clinics we work with have images interpreted daily so that the final report can be given to the patient. You have the freedom to choose your course of action based on your mission and vision.
Concerning our routine ultrasound report procedure, we need to answer the questions:
- Do they jeopardize patient safety?
- Are they legally defensible?
- Would they put our reputation at risk if widely known?
Our patients feel an urgency to have definitive information about their pregnancy. They need their confirmed diagnosis, not the nurse's preliminary findings.
My nightmare concerning delays in the physician reading Dove Medical's ultrasound exams is that our nurse will miss an ectopic pregnancy the physician would have caught, the patient will not have received the appropriate instructions and/or referral for immediate care, and the patient will suffer injury as a result. I strive to insure both the skill level of our nurses and also the prompt reading of all exams.
Should We or Shouldn't We?
While some Medical Directors feel it would be consistent with the highest level of care which we strive for, that these standards should be recommended/set and then the center should work toward them, other Medical Directors who have discussed the issue feel strongly that we do not need to comply with the 24 hour mandate and that it would be impossible for most centers to do so.
Where the Rubber Meets the Road
We must remember that our Medical Directors are volunteering their services. If pressure is put upon them to comply with this standard, are we risking losing them as a Medical Director? If that scenario is a high probability, we must ask "How is this patient best served?" What do we tell the patient?
We can't do the sonogram because we can't turn the report around in 24 hours? Is a longer turn around period better for the patient than having no service at all? Also it is critical that we not alienate our Medical Directors who are sacrificing their time and skills to serve the patients in our clinic. Without them, we cannot offer ultrasound services at all.
If we set this as policy because it meets national standards but we cannot comply, what are the consequences? Is it better to adopt a policy set on the highest excellence we are feasibly able to provide so that we can continue serving our patients, rather than potentially losing our medical director or other consequences which would impede serving the patient? Then as we can, going forward, do what is possible to shorten the turn-around time.
Practical Considerations
Centers should make efforts to have ultrasound reports read, signed and returned within the shortest time frame that is reasonably feasible. Any scans with questionable findings of concern or emergency problems should be referred promptly to a physician or hospital emergency room. This policy should be made known to the patient on the intake form.
You may want to consider the following options, among others, as means to improve your turn-around time. This is only a sampling of options and not a recommendation of any specific option.
- Use Doc-U-Sign as a mechanism to transmit scans via internet with appropriate safeguards for patient identity.
- Both E-Kyros (www.ekyros.com) and WayCool (www.waycoolsw.com) have options available for uploading and securing the physicians signature.You may contact these businesses for more information.
- Some centers are using an encrypted cloud-based means of submitting their ultrasound reports to their physician or radiologist for review and signature.
- E-mailing the reports to the Medical Director using only a client number.
- Some ultrasound machines have a software program already installed that is capable of electronic transfer.
- Logmein is being used by some centers. This allows the Medical Director or Radiologist to log in to your computer via remote access from anywhere to sign reports. This requires transferring the images from your machine to your computer and either typing the report or scanning it in.
- Some centers upload scans to a memory stick, transfer them to the computer and use High Tail to send the ultrasound and reports to the Medical Director.
Consideration for Your Center
Inform your Medical Director of the recommendation by the AIUM and have a conversation with them. Let him/her know that it is a practice standard, not law. Discuss the best and most feasible policy for your center. Examine your current policy and practice – how well is that working? Does it meet the goal for the best service your clinic can provide for the patient? Look at and discuss some of the options for improving the turn-around time. Are there any steps you feel you should take at this time? Set a time to re-examine and evaluate.
General Ultrasound Checkup
The AIUM Official Statement concerning Limited Obstetric Ultrasound (LOU), reaffirmed on 4/2/2014, makes some clear statements about the services we provide. I am reminded again that we must see ourselves as competent medical professionals and our services as medical diagnosis. Points of emphasis in the AIUM Official Statement include:
- "A limited obstetric ultrasound examination is performed to answer a specific, acute clinical question." In our clinical setting a standard sonogram is unnecessary. Our clinical question is "Is there a viable pregnancy?"
- "Clinical judgment should be used to determine the proper type of ultrasound examination to perform." This is why we don't perform a LOU if the patient is bleeding or cramping. It is no longer clinically appropriate. We need to be absolutely clear in our messaging and in the statements made by staff that an ultrasound exam is performed only when clinically indicated. At Dove Medical, we no longer allow patients to schedule an appointment for an ultrasound. Our nurse offers an ultrasound when indicated and will schedule the exam for a later date if necessary. The patient can refuse an ultrasound, but she cannot demand one.
- "Lack of qualification or inexperience of the sonographer/sonologist does not justify performance of a limited ultrasound examination when a standard examination is indicated." Our nurses must tell the patient we obtain only three pieces of information because that is how we answer the specific clinical question before us. This means our RNs don't tell patients that they aren't trained to do [fill in the blank – patient questions we've gotten include "Is everything all right?" "Is it a boy or girl?" etc.]
- "Obstetric ultrasound examinations are not performed for entertainment or for sex determination in the absence of an accepted clinical indication." At PMCs, we perform the LOU to make a pregnancy diagnosis and for no other purpose.
- "When a patient undergoes a limited ultrasound examination, it is important that she understands why a limited scan is being done and that she has appropriate expectations regarding the information sought." Again, we must clearly understand the clinical reason we scan, so that our messaging to our patients emphasizes our scope of practice. Our consent form must have a statement about the limited exam to determine only three pieces of information (location of pregnancy, heartbeat, gestational age) for the purpose of diagnosing pregnancy because that is our limited scope of clinical practice and the patient must sign that she understands this.
As an education organization Equip Leaders Now and Sonography Now have responsibility to keep ourselves informed of changes that may impact your specialized clinical setting. Our role is to pass information along and let you decide how it fits in your clinic. At Sonography Now, our mission is to provide education related to imaging, at Equip Leaders Now, our mission is to build leaders by providing the tools needed to make informed decisions to build strong communities. In doing this we have an obligation to give you information so you can be empowered with the information to form your own talking points and messaging so you can be represented well in your community and to the patients you serve.
Contact Connie Ambrecht or Beverly Anderson at 702-925-8737 with any questions or for a private webinar for your team on this topic.
NAPN: A Voice for Pro-Life Nurses
by Lynn Smith RN, National Association of Pro-Life Nurses Member,
and Marianne Linane RN, MS, MA, National Association of Pro-Life Nurses Executive Director
In 1995, during the U.S. Senate debate on the Partial-Birth Abortion Ban Act, Sen. Barbara Boxer (D. California) read into the record a letter from Geri Marrullo, then-executive director of the American Nurses Association, in opposition to the proposed ban on Partial-Birth Abortion.
The ANA claimed to be "the only full-time professional organization representing the nation's 2.2 million registered nurses."
While investigating the ANA's exclusive claim to represent the nation's RNs to the U.S. Senate, it was discovered that though there were 2.2 million RNs at the time, and the ANA is exclusively RNs, only 190,000 nurses were actually members; only 9% of U.S. nurses.
In 2011, there were 3.1 million nurses, and only 180,000 nurses were members, or about 6%.
RN Magazine, the mainstream nursing journal, did a survey in 1999, showing that nearly 2/3 of nurses surveyed thought that partial-birth abortion should be prohibited by law. [Marissa Ventura RN, Aug. 16, 2002, "Ethics on the Job: Where Nurses Stand on Abortion."]
In response to the ANA's position against a ban, a unique and separate professional nurses organization, the National Association of Pro-Life Nurses stepped forward and, in 2000, submitted a Friend of the Court brief in Stenberg v. Carhart, supporting a ban on partial birth abortion. In 2003, NAPN nurses gathered nurses' signatures on a national petition, which was submitted to the U.S. Congress, also to ban the procedure.
All nurses can appreciate the gains that the ANA has accomplished in making nursing more professional and patient care more effective. This is what we want and expect from a full-time professional association.
If the ANA was only neutral on bioethical issues, we would have cause for concern, but the clearly aggressive anti-life political lobbying by the ANA, is a disservice to nurses of conscience, and a misrepresentation to the public, to our courts, to our elected officials, and even to other nurses.
NAPN
The National Association of Pro-Life Nurses offers nurses of conscience a choice for affiliation with a professional organization that is a voice affirming the gift of life.
Chartered since 1978, The National Association of Pro-Life Nurses is a not-for-profit organization uniting nurses who are "dedicated to promoting respect for every human life from conception to natural death, and to affirming that the destruction of that life, for whatever reason and by whatever means, does not constitute good nursing practice."
It's a community of like-minded nurses who can offer advice and encouragement on problems that nurses encounter.
As a professional organization, NAPN works to:
- establish and protect the ethical values of the nursing profession.
- secure protection of the rights of nurses and paramedical personnel, who refuse to participate in procedures that are counter to the beliefs held in the NAPN mission statement.
- maintain a legal defense fund for use in representing nurses in such disputes.
- participate in the legislative process to promote life-affirming legislation.
The NAPN legal defense fund also provides the resources needed to submit Friend of the Court briefs in cases such as those heard by the United States Supreme Court. Several of these briefs have been filed, some which are on the opposite side of the argument from the American Nurses Association's briefs, such as Stenberg v. Carhart and the more recent decision, Hobby Lobby v. Sebelius.
Education
NAPN provides education for those facing difficult choices involving life-taking decisions and promotion of positive alternative choices.
Members are kept informed on current issues through Pulse Line, the quarterly newsletter, and links to relevant medical journal articles at the website: NursesForLife.org.
A $1,000 scholarship is awarded annually to a nursing student whose application best meets the criteria established. It is decided by the scholarship committee.
Continuing education is provided at its general meetings, in conjunction with the annual National Right to Life Committee Convention and speakers are provided for local nursing events on life topics.
NAPN has a strong position statement supporting informed consent for human research subjects.
Two outstanding pro-life nurses who have been members are Brenda Pratt Shafer, the nurse who exposed the practices at Martin Haskell's abortion clinic, because she was an eyewitness to partial-birth abortions, and Jill Stanek, who exposed the practice of abandoning babies surviving late-term abortions, left to die, alone and uncomforted, in the dirty utility room of the hospital where she worked.
Both Brenda and Jill have testified before the U.S. Congress and both were instrumental in having those practices outlawed, to the extent that Congress could act.
For more information visit NursesForLife.org Consider becoming a member of the National Association of Pro-Life Nurses, and joining your voice with the professional organization that can best represent your life affirming values to other nurses, to the public, to our courts and to our elected representatives.
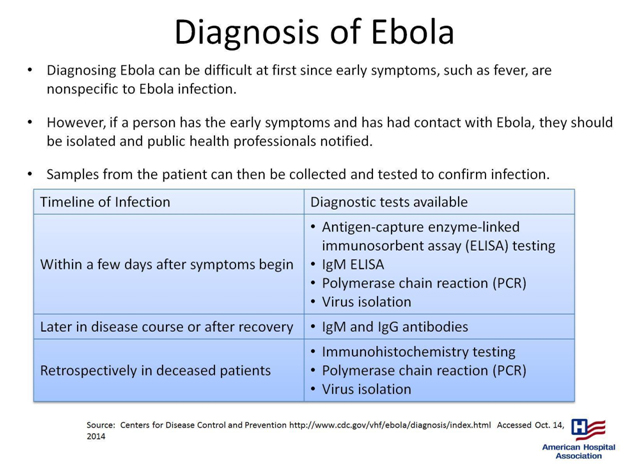
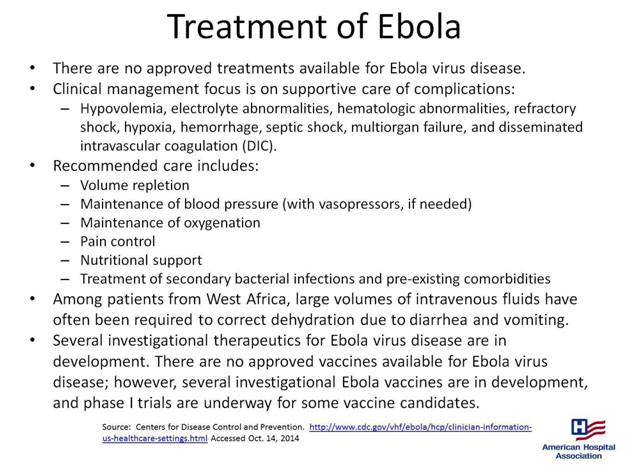
Ebola 101

by Susan Dammann RN, Medical Specialist
With the recent presentation of Ebola cases in the United States, many in the health care field, including pregnancy center staff, are seeking to learn more about the virus and even more so, if prevention measures should be put into place. This article is intended as a resource to help you achieve those goals.
Part 1 will familiarize you with information about the Ebola virus, risks of transmission, symptoms of Ebola infection, and the diagnosis and treatment of Ebola victims, not inclusive of hospital protocol. Part 2 will offer recommendations and tools from various sources your center may wish to use to develop guidelines and procedures to screen for and deal with possible Ebola carriers.
Part 1: Information
Ebola, also known as Ebola hemorrhagic fever, is a severe viral illness that is rare and can be deadly. It is caused by an infection with one of the Ebola virus strains. To date, there have been nearly 9,000 reported cases of infection with Ebola in Africa in the recent outbreak, with more than 4,000 of those cases resulting in death.
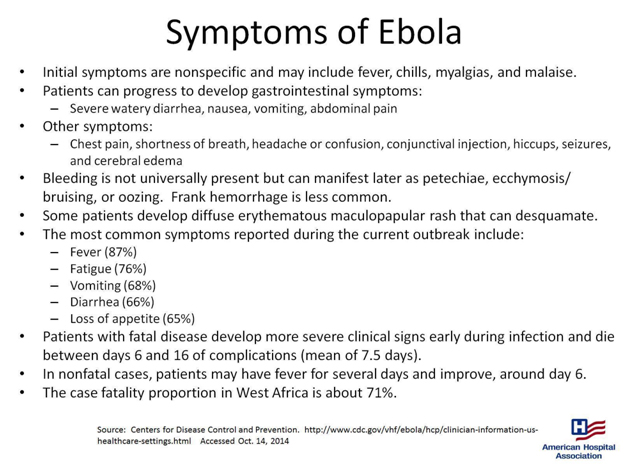
- "One of the difficulties in identifying potential cases of Ebola infection is the nonspecific presentation of most patients. Fever/chills and malaise are usually the initial symptoms, so all medical personnel should maintain a high index of suspicion in these cases.
- Patients who survive infection with Ebola generally begin to improve around day 6 of the infection.
- There is no cure for Ebola infection; treatment is largely supportive. Therefore, prevention of the spread of Ebola in healthcare facilities is particularly important.
- Patients with fever, even subjective fever, or other symptoms associated with Ebola infection along with a history of travel to an Ebola-affected area within the past 21 days need to be identified in triage.
- If such a patient is identified, she/he needs to be isolated immediately in a single room with access to a bathroom. The door to the room should remain closed." (quoted from MedScape.org)

Transmission
"When an infection does occur in humans, the virus can be spread in several ways to others. Ebola is spread through direct contact (through broken skin or mucous membranes in, for example, the eyes, nose, or mouth) with
- blood or body fluids (including but not limited to urine, saliva, sweat, feces, vomit, breast milk, and semen) of a person who is sick with Ebola
- objects (like needles and syringes) that have been contaminated with the virus
- infected fruit bats or primates (apes and monkeys)
Once someone recovers from Ebola, they can no longer spread the virus. However, Ebola virus has been found in semen for up to 3 months. Abstinence from sex (including oral sex) is recommended for at least 3 months. If abstinence is not possible, condoms may help prevent the spread of disease."
(quoted from cdc.gov)
"Persons who have direct contact with infected individuals or their blood and body fluids, such as healthcare personnel without access to appropriate personal protective equipment or other caregivers in hospitals or homes, and persons handling bodies of deceased EVD patients are at high risk for Ebola virus exposure and infection.
Airborne transmission of Ebola virus has been hypothesized but not demonstrated in humans. While Ebola virus can be spread through airborne particles under experimental conditions in animals, this type of spread has not been documented during human EVD outbreaks in settings such as hospitals or households.
CDC infection control recommendations for U.S. hospitals, including recommendations for standard, contact, and droplet precautions for general care, reflect the established routes for human-to-human transmission of EVD and are based on data collected from previous EVD outbreaks in Africa in addition to experimental data."
(quoted from cdc.gov)
Can Ebola Be Transmitted Through a Sneeze?
"The only time that Ebola is in the lungs in sufficient quantities to produce virus in fluid that would be expelled during a sneeze is during extraordinarily advanced disease. A typical Ebola patient doesn't have a lot of virus in the lungs, but a person with advanced disease who is close to death could have a lot of virus in the lungs. During intubation, or when a very sick, infected person coughs or sneezes, an improperly protected healthcare worker could be at risk for being infected.
It would be a stretch to say that someone who is infected but well enough to walk around among other people would have enough Ebola in his or her lungs to be able to spread it by sneezing."
(quoted from MedScape.org)
Part 2: Recommendations and Tools
Pregnancy Center Considerations
If your center is currently serving clients from West African countries where the Ebola Virus has been reported, then you may wish to consider proactively creating a screening policy.
Should Ebola become a serious concern in our nation, the following are recommendations from various sources. Your board of directors in conjunction with your Medical Director or Medical Advisor may then need to develop the best strategy for your center in screening for Ebola carriers and what protocol your center will follow should such a person be identified.
Medscape interviewed Arjun Srinivasan, MD (CAPT, USPHS), Associate Director of CDC's Division of Healthcare Quality Promotion, asking some key questions about the Ebola crisis. They began with the upcoming influenza season and the worries that primary care clinicians may have about symptomatic patients who also have concerns about Ebola.
"Medscape: How should clinicians handle patients who present with symptoms of fever, nausea, and vomiting, in light of current Ebola recommendations?
Arjun Srinivasan, MD (CAPT, USPHS): It's important to remember that the telephone can be one of the tools that can help keep us safe from Ebola. When people call for appointments, it's an opportunity to ask them the screening questions about whether they might have risks for Ebola. Important in that is a travel history or potential exposure to a patient with Ebola. A checklist for patients being evaluated for Ebola is available on the CDC website.
Medscape: If there is no positive travel or exposure history in the past 21 days, can a clinician rule out Ebola?
Dr Srinivasan: Yes. The exposure or travel history is a key to identifying patients who might be infected with Ebola. There is an algorithm you can use to help you determine who might be at risk for Ebola, available at cdc.gov."
(quoted from MedScape.com)
The CDC Checklist for Patients Being Evaluated for Ebola Virus Disease (EVD) in the United States (linked to above) may offer some initial steps upon arrival of a possible carrier and initial assessment.
Below are three protocols and a questionnaire from the Franklin County, Ohio Health Department website. (Heartbeat International is located in Franklin County, Ohio) You may also want to look on the health department websites in your county for their recommendations.
Protocol for Assessing Possible Ebola Exposure in Healthcare Settings
Protocols for Dispatch and First Responders to Limit Exposure to Ebola
Protocol for Assessing Possible Ebola Exposure in Work Settings
Travel History and Exposure Screening Questionnaire
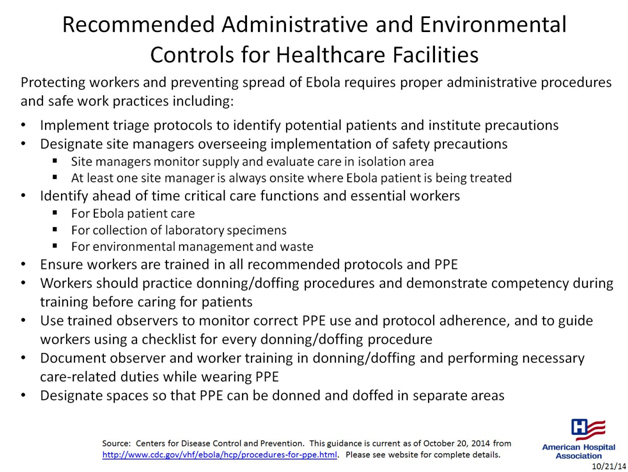
From the following document by the American Hospital Association the following may be of importance:
- Implement triage protocols to identify potential patients and institute precautions
- Designate site managers overseeing implementation of safety precautions
.
The following statements from the CDC may be helpful as you consider what steps to take.
"When a patient possibly infected with the Ebola virus appears in a hospital emergency department (ED), clinicians need not necessarily cover themselves from head to toe with personal protective equipment (PPE), according to new guidelines from the Centers for Disease Control and Prevention (CDC).
The CDC also emphasizes that ED patients with an unconfirmed Ebola infection are not contagious unless they are vomiting, bleeding, having diarrhea, or otherwise producing body fluids associated with an advanced stage of the disease and a healthcare worker comes in direct contact with them.
"If you're not at risk of being exposed to blood or body fluids, then you're not at risk of transmission," said Arjun Srinivasan, MD, associate director of the healthcare-associated infection prevention programs of the CDC's National Center for Emerging and Zoonotic Infectious Diseases. "When that risk exists — the patient is throwing up, for example — then you choose PPE that provides full-scale protection."
The first step in the CDC's algorithm for ED clinicians is determining the patient's exposure history: Has he or she lived in or traveled to a country with widespread Ebola disease or had contact with an infected person in the previous 21 days? If so, then the identification of Ebola signs or symptoms comes next. One sign is fever, either subjective or 100.4°F and higher. Other signs include headache, weakness, and muscle pain, as well as the red-alert symptoms of vomiting, diarrhea, abdominal pain, and hemorrhage, as in bleeding gums or nose bleeds.
A patient with these signs and symptoms along with a definite exposure history should be isolated immediately, either in a private room or a separate enclosed area with a private bathroom or a covered bedside commode. The CDC guidance states that only essential healthcare workers with designated roles should care for the patient and should log in and out of the room.
More information on the new Ebola guidance from the CDC is available on the agency's website.
(quoted from MedScape.com)
For additional or ongoing information, the CDC has a wealth of information available here.
Above all, we must look in faith to God Almighty for His wisdom and protection. Psalm 91 is a magnificent promise of protection and there is no better time for daily meditation in this Psalm, as we rest in faith in the One who is able to keep us safe in times of trouble.
How Your Center Can Help Prevent Ebola's Spread

As the Ebola outbreak has spread from West Africa to isolated cases in parts of Europe and now the United States, there has been no shortage of panic and paranoia among Westerners—even those working in the health care fields.
Still, it is an established and repeated fact that Ebola's spread can be prevented simply by following proper safety procedures in a medical setting. An informational page on Ebola published at the World Health Organization's (WHO) website points to the sad reality of Ebola's largely preventable spread:
Health-care workers have frequently been infected while treating patients with suspected or confirmed EVD [Ebola Virus Disease]. This has occurred through close contact with patients when infection control precautions are not strictly practiced.1
As those involved in the life-saving work of pregnancy help in the medical setting, how can you protect yourself, your clinic, and your clients from this deadly virus?
The answer starts with educating yourself, your staff and volunteers, and your clients as to how Ebola spreads, which, again according to WHO, involves the following:
Ebola... spreads through human-to-human transmission via direct contact (through broken skin or mucous membranes) with the blood, secretions, organs or other bodily fluids of infected people, and with surfaces and materials (e.g. bedding, clothing) contaminated with these fluids.2
Consider the functions of your Pregnancy Help Medical Center or Clinic.
- Could you come into contact with any bodily fluid when handling a urine pregnancy test?
- What about collecting a specimen for STD/STI testing?
- Broken skin that can be exposed and contacted while conducting an ultrasound?
With these points of contact posing risks in light of the Ebola virus—in addition to several diseases that are much more likely to spread—make sure your center is paying special attention to policies such as Universal Precautions as defined by the Centers for Disease Control (CDC) and OSHA Regulations.
Under Universal Precautions, blood and certain body fluids of all patients are considered potentially infectious for HIV, (Hepatitis B), and other blood-borne pathogens. Universal Precautions involve the routine wearing of gloves, other protective clothing, hand washing, and such infection control measures that are designed to place a barrier between potentially infectious blood or body fluids and employees.3
For more information on how you can keep your center protected from the spread of viral infection, check out Heartbeat International's Medical Essentials for Pregnancy Help Organizations©.
1. "Ebola virus disease," World Health Organization, http://www.who.int/mediacentre/factsheets/fs103/en/ (accessed Oct. 17, 2014).
2. Ibid.
3. Medical Essentials for Pregnancy Help Organizations©, Heartbeat International, 2014, Part IV, page 4.