Jennifer Wright
2015: Start Now on Long-Term Success
by Kirk Walden, Advancement Specialist
A successful, effective advancement plan is not an overwhelming task; nor is it one that requires extraordinary fundraising skill.
Frankly, a winning plan for raising funds and advancing the ministry to a new tier is all about consistency and . . . Smart planning that is based on incremental improvement.
Here is what I mean:
Often we look at our finances and declare, "We need another event" or, "We must make major improvements in this area or that one in order to raise these funds!" On the idea of another event, in this issue we will blow that myth out of the water. If your ministry has two events, you have plenty. A third can actually be a detriment to a winning plan.
And when it comes to "major" gains in fundraising, most of the time we will find that it is step-by-step, small improvements that make the biggest difference to our overall success. This month, let's take a look at seemingly slight changes that can bring us powerful results, over time.
If we look long-term, we will find three avenues for success:
Evaluate
Time spent evaluating our current fundraising plan is always time well spent. Give our events a second, and third, look. Let's make sure each event is a wise use of our time.
Plan
Space events, appeal letters and in-person asks so that we are not constantly in an overwhelmed rush. Back-to-back events burn out all of us. And running an event (such as a baby bottle campaign) nearly year-round never gives us a chance to breathe.
Focus on the long term
Implement long term funding streams such as building monthly support and regularly meeting with those who can give major gifts, setting up your ministry for success long into the future.
For instance, did you know that adding just two $40/month donors each month will result in more than $55,000 in yearly funding over five years? That's success. Check out other articles in this month's issue that show us the way to a winning development plan, in good time.
Click here for more of this month's Advancement Trends in the Life Community.
Arranging Adoptions
 In 1944, Marguerite Bonnema received the shock of her life.
In 1944, Marguerite Bonnema received the shock of her life.
To her surprise, a little neighbor girl revealed her father's strong dislike of his wife's illegitimate baby girl. "He is going to kill [the baby]," the little girl said. Marguerite replied, "Tell him not to kill her but to give her to me."
Arrangements were made - in a hurry. The neighbor mother and baby girl traveled by bus to a train station, where Marguerite and her friend and roommate Mary DeBoer received the child to live with them in their small apartment.
Since then, Bethany Christian Services has been following in these two co-founders' steps, demonstrating the love and compassion of Jesus Christ to expectant parents who are facing an unplanned pregnancy and need help. Our goal is to help them explore their life-affirming options and then help them pursue the plan they decide is best for themselves and their baby—whether that is parenting or adoption.
As a Heartbeat International partner, it is our desire to share our pregnancy counseling resources with those who are ministering to expectant parents in resource centers across the U.S.
Our full range of informational resources include brochures, books, DVDs, and educational webinars (some available in Spanish). As a resource to clients, our Lifeline staff is also available to chat online or by phone at 1.800.238.4269. We want to work with you to help bring hope, information, and services to expectant parents in crisis—meeting them anytime and anywhere.
For more information or to order any resources, please visit Bethany.org/Store.
Who is the Person You Need to Encourage?
by Kirk Walden, Advancement Specialist
"But encourage one another day after day, as long as it is still called 'today,' so that none of you will be hardened by the deceitfulness of sin."
Hebrews 3:13

None of us wants to be involved in sin. It's an ugly thing and as Christians we certainly want to avoid whatever it is that tempts us. Still, in the real world, avoiding sin is not easy.
What would we do if there were a "sin shot" we could take that would shield us from falling into vicious anger, gossip, hatred or any one of the sins that can so easily overtake our minds?
What if someone came up to us and said, "Here's the vaccine; take this and if you continue with regular doses and up the medication when temptation comes, you'll likely avoid doing wrong altogether!"?
Would I take that shot? Yep . . . And the writer of Hebrews gives us our "Sin Antidote" in Hebrews 3:13. The antidote is simple - encouragement.
The writer here is not giving us a nice phrase to remember, but a proven fact for the Christian: Spend your day encouraging, and sin will flee your mind and your actions. The hardened heart you fear will never be a problem for you.
Often I can see the word "encourage" as only icing on the Christian cake - a nice addition to the walk of faith, but nothing to get too excited about. Yet that's not what the writer of Hebrews is saying. To the writer, encouragement is essential.
Shifting my thinking, I need to see encouragement as an integral part of every day in my life. Who have I encouraged today? And how? Who needs encouragement?
The writer's point I believe, is this: When we make encouragement a daily focus, we no longer have time for temptation—or yielding to temptations. Encouragement builds relationships, and builds up a foundation for a stronger Body of Christ.
So take heart. Today is the day to encourage. When we do, our hearts remain soft and our ability to be mighty in the faith becomes strong.
Fuss about Practice Fusion?
By Jor-El Godsey, Vice President
If you don't know the difference between EHR and EMR and PHR, HIPAA and HI-TECH, EPM and PMS , PRC and PMC, then stop reading.
If you do, or think you do, you're probably knee-deep in medical clinic regulations and/or clinic practices.
Pregnancy help medical clinics have been growing in number and complexity for the last twenty years. Originally focused on ultrasound services, many life-affirming, medically savvy centers are expanding medical services to include STI testing/treatment, pre-natal care, and more.
Good business systems, important for all pregnancy help organizations, has been a dynamic question for medically focused affiliates with the changing nature of health care regulations.
Life-affirming friends like eKyros and WayCool that specialize in database solutions for pregnancy help organizations have been answering that question with increased security, encrypted records and other HIPAA-necessary implementations. However, some in our community have either opted for, or promoted other software.
One of those is Practice Fusion. And, yes, there has been a fuss about Practice Fusion.
Practice Fusion is presented as being "free" (always attractive to non-profits) and, despite its relative newness (launched in 2007), has been quickly accepted by doctors office across the U.S. There are, however, some troubling findings that ought to give life-affirming pregnancy help organizations pause.
First, is anything really "free"? The article, "What Makes Free EHRs Expensive in the Long Run?" rightly notes, "...hidden expenses, heightened risk and unforeseen liabilities can cost you just as much as any web-based EHR..." So always beware of any Open Source product being offered for FREE.
Second, venture capitalists have invested nearly $200 million in this product. How will they realize their return on investment? It's always good to look a little closer to understand how a free product is able to remain current, supported and adaptable for future innovation. An article from Business Week notes the following:
The company makes money by charging more than 70,000 pharmacies, 300 diagnostics labs, and 21 imaging centers for access to its captive community of medical pros. For example, labs pay for the convenience of transmitting test results rather than faxing them, while drugmakers pay to deliver targeted ads to doctors. For an additional fee, companies can use a Practice Fusion tool to sift through its trove of more than 80 million patient records to identify patterns, such why doctors might be choosing one drug over another. The data is stripped of any information that would reveal the identity of the patients. The company is also working with insurer Aetna (AET) to identify at-risk patients to head off costly trips to the emergency room.
A pregnancy help organization using Practice Fusion apparently becomes part of the "captive community" targeted by those profiting from offering this "free" product.
Third, Practice Fusion's own practices have created significant compliance and confidentiality questions. Some industry watchers have noted, that "[a]ccording to experts, it may have violated the grand poobah of medical privacy laws — HIPAA — potentially getting both the doctors and Practice Fusion — as a "business associate" — into trouble. Additionally, the Federal Trade Commission may see what the start-up did as a deceptive business practice."
Along with these three specific points about Practice Fusion (or free EHRs in general), there comes a much more basic question:
Is there value in working within our specialized world of life-affirming pregnancy help to sharpen a good tool for all of us to use?
We think so, and we encourage you to think carefully when considering such important business tools.
24 Hour Turn-Around on Ultrasound Scans?
Making Sense of AIUM Guidelines
Connie Ambrecht RDMS, Executive Director Equip Leaders Now/Sonography Now
Beverly Anderson, J.D., CEO Dove Medical
Susan Dammann RN LASm Medical Specialist
The Issue
In April 2014, the American Institute of Ultrasound in Medicine (AIUM) sent an email to its members stating it had "Updated Guidelines and Official Statements." Included in the list was the guideline titled "Documentation of an Ultrasound Examination."
First, it is valuable to revisit who AIUM is, as well as its role in ultrasound imaging. In its own words, "the AIUM is an association dedicated to advancing the safe and effective use of ultrasound in medicine through professional and public education, research, development of guidelines, and accreditation."
In the first section of the guidelines, AIUM outlines what it considers high-quality patient care. The guidelines state a permanent record should always be kept of the images, and an interpretation should be provided for patient records. All medical professionals involved should be able to communicate well and work as a team to provide what is expected: quality patient care.
The next section lists what should be included in the official report. In some clinical settings, the interpretation of the images is transcribed and a separate report page is generated for the patients chart. In the PMC setting it is common that a signature is obtained on the ultrasound report page and serves as the final report.
Section three discusses the final report from the interpreting physician or medical director of the clinic. According to this April 2014 update, the final report should be generated in 24 hours. I know you are thinking or asking... "How can we do that?!"
We restate the following from the AIUM guideline: Practice guidelines of the AIUM are intended to provide the medical ultrasound community with guidelines for the performance and recording of high-quality ultrasound examinations. The guidelines reflect what the AIUM considers the minimum criteria for a complete examination in each area but are not intended to establish a legal standard of care.
This AIUM Guideline is NOT a legal requirement. It is a national practice standard.
We at Sonography Now live in the service trenches with you as we train on-site. We understand that getting interpretations in a timely fashion versus every 24 hours can seem unnecessary. Taking one step at a time can ease such a transition. If you want to make changes to accommodate a faster interpretation time, it doesn't need to change immediately.
Building a plan of action can remedy the feeling of urgency. Some clinics we work with have images interpreted daily so that the final report can be given to the patient. You have the freedom to choose your course of action based on your mission and vision.
Concerning our routine ultrasound report procedure, we need to answer the questions:
- Do they jeopardize patient safety?
- Are they legally defensible?
- Would they put our reputation at risk if widely known?
Our patients feel an urgency to have definitive information about their pregnancy. They need their confirmed diagnosis, not the nurse's preliminary findings.
My nightmare concerning delays in the physician reading Dove Medical's ultrasound exams is that our nurse will miss an ectopic pregnancy the physician would have caught, the patient will not have received the appropriate instructions and/or referral for immediate care, and the patient will suffer injury as a result. I strive to insure both the skill level of our nurses and also the prompt reading of all exams.
Should We or Shouldn't We?
While some Medical Directors feel it would be consistent with the highest level of care which we strive for, that these standards should be recommended/set and then the center should work toward them, other Medical Directors who have discussed the issue feel strongly that we do not need to comply with the 24 hour mandate and that it would be impossible for most centers to do so.
Where the Rubber Meets the Road
We must remember that our Medical Directors are volunteering their services. If pressure is put upon them to comply with this standard, are we risking losing them as a Medical Director? If that scenario is a high probability, we must ask "How is this patient best served?" What do we tell the patient?
We can't do the sonogram because we can't turn the report around in 24 hours? Is a longer turn around period better for the patient than having no service at all? Also it is critical that we not alienate our Medical Directors who are sacrificing their time and skills to serve the patients in our clinic. Without them, we cannot offer ultrasound services at all.
If we set this as policy because it meets national standards but we cannot comply, what are the consequences? Is it better to adopt a policy set on the highest excellence we are feasibly able to provide so that we can continue serving our patients, rather than potentially losing our medical director or other consequences which would impede serving the patient? Then as we can, going forward, do what is possible to shorten the turn-around time.
Practical Considerations
Centers should make efforts to have ultrasound reports read, signed and returned within the shortest time frame that is reasonably feasible. Any scans with questionable findings of concern or emergency problems should be referred promptly to a physician or hospital emergency room. This policy should be made known to the patient on the intake form.
You may want to consider the following options, among others, as means to improve your turn-around time. This is only a sampling of options and not a recommendation of any specific option.
- Use Doc-U-Sign as a mechanism to transmit scans via internet with appropriate safeguards for patient identity.
- Both E-Kyros (www.ekyros.com) and WayCool (www.waycoolsw.com) have options available for uploading and securing the physicians signature.You may contact these businesses for more information.
- Some centers are using an encrypted cloud-based means of submitting their ultrasound reports to their physician or radiologist for review and signature.
- E-mailing the reports to the Medical Director using only a client number.
- Some ultrasound machines have a software program already installed that is capable of electronic transfer.
- Logmein is being used by some centers. This allows the Medical Director or Radiologist to log in to your computer via remote access from anywhere to sign reports. This requires transferring the images from your machine to your computer and either typing the report or scanning it in.
- Some centers upload scans to a memory stick, transfer them to the computer and use High Tail to send the ultrasound and reports to the Medical Director.
Consideration for Your Center
Inform your Medical Director of the recommendation by the AIUM and have a conversation with them. Let him/her know that it is a practice standard, not law. Discuss the best and most feasible policy for your center. Examine your current policy and practice – how well is that working? Does it meet the goal for the best service your clinic can provide for the patient? Look at and discuss some of the options for improving the turn-around time. Are there any steps you feel you should take at this time? Set a time to re-examine and evaluate.
General Ultrasound Checkup
The AIUM Official Statement concerning Limited Obstetric Ultrasound (LOU), reaffirmed on 4/2/2014, makes some clear statements about the services we provide. I am reminded again that we must see ourselves as competent medical professionals and our services as medical diagnosis. Points of emphasis in the AIUM Official Statement include:
- "A limited obstetric ultrasound examination is performed to answer a specific, acute clinical question." In our clinical setting a standard sonogram is unnecessary. Our clinical question is "Is there a viable pregnancy?"
- "Clinical judgment should be used to determine the proper type of ultrasound examination to perform." This is why we don't perform a LOU if the patient is bleeding or cramping. It is no longer clinically appropriate. We need to be absolutely clear in our messaging and in the statements made by staff that an ultrasound exam is performed only when clinically indicated. At Dove Medical, we no longer allow patients to schedule an appointment for an ultrasound. Our nurse offers an ultrasound when indicated and will schedule the exam for a later date if necessary. The patient can refuse an ultrasound, but she cannot demand one.
- "Lack of qualification or inexperience of the sonographer/sonologist does not justify performance of a limited ultrasound examination when a standard examination is indicated." Our nurses must tell the patient we obtain only three pieces of information because that is how we answer the specific clinical question before us. This means our RNs don't tell patients that they aren't trained to do [fill in the blank – patient questions we've gotten include "Is everything all right?" "Is it a boy or girl?" etc.]
- "Obstetric ultrasound examinations are not performed for entertainment or for sex determination in the absence of an accepted clinical indication." At PMCs, we perform the LOU to make a pregnancy diagnosis and for no other purpose.
- "When a patient undergoes a limited ultrasound examination, it is important that she understands why a limited scan is being done and that she has appropriate expectations regarding the information sought." Again, we must clearly understand the clinical reason we scan, so that our messaging to our patients emphasizes our scope of practice. Our consent form must have a statement about the limited exam to determine only three pieces of information (location of pregnancy, heartbeat, gestational age) for the purpose of diagnosing pregnancy because that is our limited scope of clinical practice and the patient must sign that she understands this.
As an education organization Equip Leaders Now and Sonography Now have responsibility to keep ourselves informed of changes that may impact your specialized clinical setting. Our role is to pass information along and let you decide how it fits in your clinic. At Sonography Now, our mission is to provide education related to imaging, at Equip Leaders Now, our mission is to build leaders by providing the tools needed to make informed decisions to build strong communities. In doing this we have an obligation to give you information so you can be empowered with the information to form your own talking points and messaging so you can be represented well in your community and to the patients you serve.
Contact Connie Ambrecht or Beverly Anderson at 702-925-8737 with any questions or for a private webinar for your team on this topic.
NAPN: A Voice for Pro-Life Nurses
by Lynn Smith RN, National Association of Pro-Life Nurses Member,
and Marianne Linane RN, MS, MA, National Association of Pro-Life Nurses Executive Director
In 1995, during the U.S. Senate debate on the Partial-Birth Abortion Ban Act, Sen. Barbara Boxer (D. California) read into the record a letter from Geri Marrullo, then-executive director of the American Nurses Association, in opposition to the proposed ban on Partial-Birth Abortion.
The ANA claimed to be "the only full-time professional organization representing the nation's 2.2 million registered nurses."
While investigating the ANA's exclusive claim to represent the nation's RNs to the U.S. Senate, it was discovered that though there were 2.2 million RNs at the time, and the ANA is exclusively RNs, only 190,000 nurses were actually members; only 9% of U.S. nurses.
In 2011, there were 3.1 million nurses, and only 180,000 nurses were members, or about 6%.
RN Magazine, the mainstream nursing journal, did a survey in 1999, showing that nearly 2/3 of nurses surveyed thought that partial-birth abortion should be prohibited by law. [Marissa Ventura RN, Aug. 16, 2002, "Ethics on the Job: Where Nurses Stand on Abortion."]
In response to the ANA's position against a ban, a unique and separate professional nurses organization, the National Association of Pro-Life Nurses stepped forward and, in 2000, submitted a Friend of the Court brief in Stenberg v. Carhart, supporting a ban on partial birth abortion. In 2003, NAPN nurses gathered nurses' signatures on a national petition, which was submitted to the U.S. Congress, also to ban the procedure.
All nurses can appreciate the gains that the ANA has accomplished in making nursing more professional and patient care more effective. This is what we want and expect from a full-time professional association.
If the ANA was only neutral on bioethical issues, we would have cause for concern, but the clearly aggressive anti-life political lobbying by the ANA, is a disservice to nurses of conscience, and a misrepresentation to the public, to our courts, to our elected officials, and even to other nurses.
NAPN
The National Association of Pro-Life Nurses offers nurses of conscience a choice for affiliation with a professional organization that is a voice affirming the gift of life.
Chartered since 1978, The National Association of Pro-Life Nurses is a not-for-profit organization uniting nurses who are "dedicated to promoting respect for every human life from conception to natural death, and to affirming that the destruction of that life, for whatever reason and by whatever means, does not constitute good nursing practice."
It's a community of like-minded nurses who can offer advice and encouragement on problems that nurses encounter.
As a professional organization, NAPN works to:
- establish and protect the ethical values of the nursing profession.
- secure protection of the rights of nurses and paramedical personnel, who refuse to participate in procedures that are counter to the beliefs held in the NAPN mission statement.
- maintain a legal defense fund for use in representing nurses in such disputes.
- participate in the legislative process to promote life-affirming legislation.
The NAPN legal defense fund also provides the resources needed to submit Friend of the Court briefs in cases such as those heard by the United States Supreme Court. Several of these briefs have been filed, some which are on the opposite side of the argument from the American Nurses Association's briefs, such as Stenberg v. Carhart and the more recent decision, Hobby Lobby v. Sebelius.
Education
NAPN provides education for those facing difficult choices involving life-taking decisions and promotion of positive alternative choices.
Members are kept informed on current issues through Pulse Line, the quarterly newsletter, and links to relevant medical journal articles at the website: NursesForLife.org.
A $1,000 scholarship is awarded annually to a nursing student whose application best meets the criteria established. It is decided by the scholarship committee.
Continuing education is provided at its general meetings, in conjunction with the annual National Right to Life Committee Convention and speakers are provided for local nursing events on life topics.
NAPN has a strong position statement supporting informed consent for human research subjects.
Two outstanding pro-life nurses who have been members are Brenda Pratt Shafer, the nurse who exposed the practices at Martin Haskell's abortion clinic, because she was an eyewitness to partial-birth abortions, and Jill Stanek, who exposed the practice of abandoning babies surviving late-term abortions, left to die, alone and uncomforted, in the dirty utility room of the hospital where she worked.
Both Brenda and Jill have testified before the U.S. Congress and both were instrumental in having those practices outlawed, to the extent that Congress could act.
For more information visit NursesForLife.org Consider becoming a member of the National Association of Pro-Life Nurses, and joining your voice with the professional organization that can best represent your life affirming values to other nurses, to the public, to our courts and to our elected representatives.
Ebola 101

by Susan Dammann RN, Medical Specialist
With the recent presentation of Ebola cases in the United States, many in the health care field, including pregnancy center staff, are seeking to learn more about the virus and even more so, if prevention measures should be put into place. This article is intended as a resource to help you achieve those goals.
Part 1 will familiarize you with information about the Ebola virus, risks of transmission, symptoms of Ebola infection, and the diagnosis and treatment of Ebola victims, not inclusive of hospital protocol. Part 2 will offer recommendations and tools from various sources your center may wish to use to develop guidelines and procedures to screen for and deal with possible Ebola carriers.
Part 1: Information
Ebola, also known as Ebola hemorrhagic fever, is a severe viral illness that is rare and can be deadly. It is caused by an infection with one of the Ebola virus strains. To date, there have been nearly 9,000 reported cases of infection with Ebola in Africa in the recent outbreak, with more than 4,000 of those cases resulting in death.
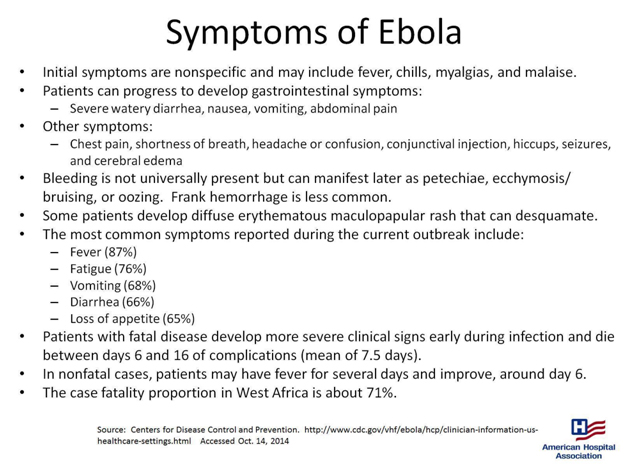
- "One of the difficulties in identifying potential cases of Ebola infection is the nonspecific presentation of most patients. Fever/chills and malaise are usually the initial symptoms, so all medical personnel should maintain a high index of suspicion in these cases.
- Patients who survive infection with Ebola generally begin to improve around day 6 of the infection.
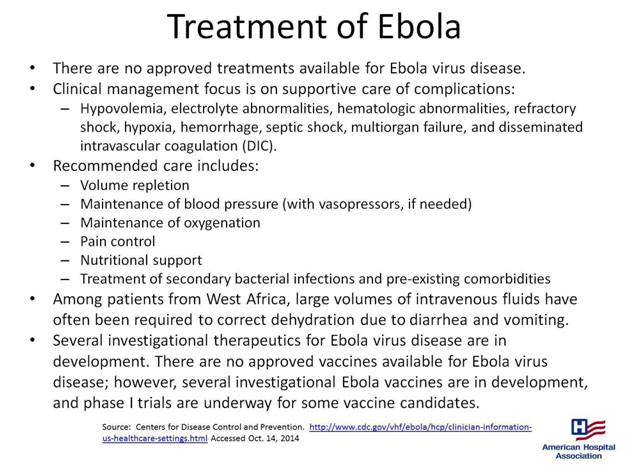
- There is no cure for Ebola infection; treatment is largely supportive. Therefore, prevention of the spread of Ebola in healthcare facilities is particularly important.
- Patients with fever, even subjective fever, or other symptoms associated with Ebola infection along with a history of travel to an Ebola-affected area within the past 21 days need to be identified in triage.
- If such a patient is identified, she/he needs to be isolated immediately in a single room with access to a bathroom. The door to the room should remain closed." (quoted from MedScape.org)

Transmission
"When an infection does occur in humans, the virus can be spread in several ways to others. Ebola is spread through direct contact (through broken skin or mucous membranes in, for example, the eyes, nose, or mouth) with
- blood or body fluids (including but not limited to urine, saliva, sweat, feces, vomit, breast milk, and semen) of a person who is sick with Ebola
- objects (like needles and syringes) that have been contaminated with the virus
- infected fruit bats or primates (apes and monkeys)
Once someone recovers from Ebola, they can no longer spread the virus. However, Ebola virus has been found in semen for up to 3 months. Abstinence from sex (including oral sex) is recommended for at least 3 months. If abstinence is not possible, condoms may help prevent the spread of disease."
(quoted from cdc.gov)
"Persons who have direct contact with infected individuals or their blood and body fluids, such as healthcare personnel without access to appropriate personal protective equipment or other caregivers in hospitals or homes, and persons handling bodies of deceased EVD patients are at high risk for Ebola virus exposure and infection.
Airborne transmission of Ebola virus has been hypothesized but not demonstrated in humans. While Ebola virus can be spread through airborne particles under experimental conditions in animals, this type of spread has not been documented during human EVD outbreaks in settings such as hospitals or households.
CDC infection control recommendations for U.S. hospitals, including recommendations for standard, contact, and droplet precautions for general care, reflect the established routes for human-to-human transmission of EVD and are based on data collected from previous EVD outbreaks in Africa in addition to experimental data."
(quoted from cdc.gov)
Can Ebola Be Transmitted Through a Sneeze?
"The only time that Ebola is in the lungs in sufficient quantities to produce virus in fluid that would be expelled during a sneeze is during extraordinarily advanced disease. A typical Ebola patient doesn't have a lot of virus in the lungs, but a person with advanced disease who is close to death could have a lot of virus in the lungs. During intubation, or when a very sick, infected person coughs or sneezes, an improperly protected healthcare worker could be at risk for being infected.
It would be a stretch to say that someone who is infected but well enough to walk around among other people would have enough Ebola in his or her lungs to be able to spread it by sneezing."
(quoted from MedScape.org)
Part 2: Recommendations and Tools
Pregnancy Center Considerations
If your center is currently serving clients from West African countries where the Ebola Virus has been reported, then you may wish to consider proactively creating a screening policy.
Should Ebola become a serious concern in our nation, the following are recommendations from various sources. Your board of directors in conjunction with your Medical Director or Medical Advisor may then need to develop the best strategy for your center in screening for Ebola carriers and what protocol your center will follow should such a person be identified.
Medscape interviewed Arjun Srinivasan, MD (CAPT, USPHS), Associate Director of CDC's Division of Healthcare Quality Promotion, asking some key questions about the Ebola crisis. They began with the upcoming influenza season and the worries that primary care clinicians may have about symptomatic patients who also have concerns about Ebola.
"Medscape: How should clinicians handle patients who present with symptoms of fever, nausea, and vomiting, in light of current Ebola recommendations?
Arjun Srinivasan, MD (CAPT, USPHS): It's important to remember that the telephone can be one of the tools that can help keep us safe from Ebola. When people call for appointments, it's an opportunity to ask them the screening questions about whether they might have risks for Ebola. Important in that is a travel history or potential exposure to a patient with Ebola. A checklist for patients being evaluated for Ebola is available on the CDC website.
Medscape: If there is no positive travel or exposure history in the past 21 days, can a clinician rule out Ebola?
Dr Srinivasan: Yes. The exposure or travel history is a key to identifying patients who might be infected with Ebola. There is an algorithm you can use to help you determine who might be at risk for Ebola, available at cdc.gov."
(quoted from MedScape.com)
The CDC Checklist for Patients Being Evaluated for Ebola Virus Disease (EVD) in the United States (linked to above) may offer some initial steps upon arrival of a possible carrier and initial assessment.
Below are three protocols and a questionnaire from the Franklin County, Ohio Health Department website. (Heartbeat International is located in Franklin County, Ohio) You may also want to look on the health department websites in your county for their recommendations.
Protocol for Assessing Possible Ebola Exposure in Healthcare Settings
Protocols for Dispatch and First Responders to Limit Exposure to Ebola
Protocol for Assessing Possible Ebola Exposure in Work Settings
Travel History and Exposure Screening Questionnaire
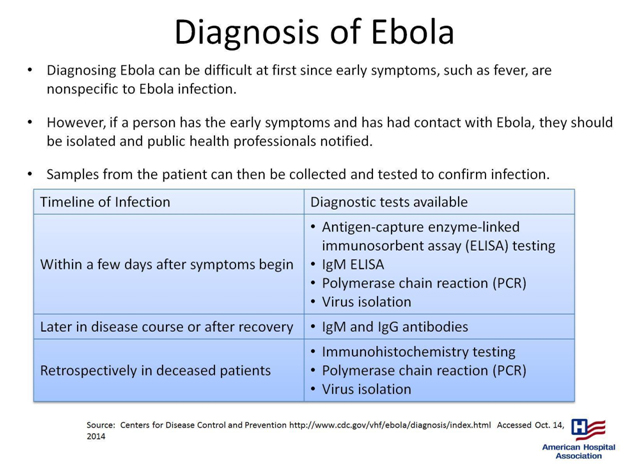
From the following document by the American Hospital Association the following may be of importance:
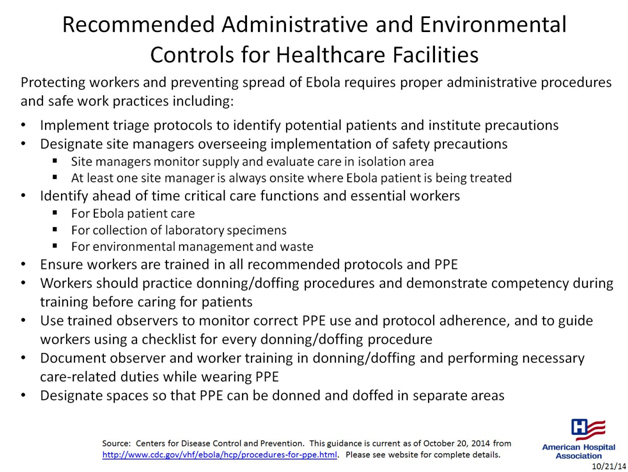
- Implement triage protocols to identify potential patients and institute precautions
- Designate site managers overseeing implementation of safety precautions
.
The following statements from the CDC may be helpful as you consider what steps to take.
"When a patient possibly infected with the Ebola virus appears in a hospital emergency department (ED), clinicians need not necessarily cover themselves from head to toe with personal protective equipment (PPE), according to new guidelines from the Centers for Disease Control and Prevention (CDC).
The CDC also emphasizes that ED patients with an unconfirmed Ebola infection are not contagious unless they are vomiting, bleeding, having diarrhea, or otherwise producing body fluids associated with an advanced stage of the disease and a healthcare worker comes in direct contact with them.
"If you're not at risk of being exposed to blood or body fluids, then you're not at risk of transmission," said Arjun Srinivasan, MD, associate director of the healthcare-associated infection prevention programs of the CDC's National Center for Emerging and Zoonotic Infectious Diseases. "When that risk exists — the patient is throwing up, for example — then you choose PPE that provides full-scale protection."
The first step in the CDC's algorithm for ED clinicians is determining the patient's exposure history: Has he or she lived in or traveled to a country with widespread Ebola disease or had contact with an infected person in the previous 21 days? If so, then the identification of Ebola signs or symptoms comes next. One sign is fever, either subjective or 100.4°F and higher. Other signs include headache, weakness, and muscle pain, as well as the red-alert symptoms of vomiting, diarrhea, abdominal pain, and hemorrhage, as in bleeding gums or nose bleeds.
A patient with these signs and symptoms along with a definite exposure history should be isolated immediately, either in a private room or a separate enclosed area with a private bathroom or a covered bedside commode. The CDC guidance states that only essential healthcare workers with designated roles should care for the patient and should log in and out of the room.
More information on the new Ebola guidance from the CDC is available on the agency's website.
(quoted from MedScape.com)
For additional or ongoing information, the CDC has a wealth of information available here.
Above all, we must look in faith to God Almighty for His wisdom and protection. Psalm 91 is a magnificent promise of protection and there is no better time for daily meditation in this Psalm, as we rest in faith in the One who is able to keep us safe in times of trouble.
Masterpieces of Life
By Jennifer Minor, Editor/Writer
For the last 42 years, October has been recognized as Respect Life Month, focusing on issues of life and the dignity of the human person, with a special emphasis each year. It's also time set aside to spread stories about the good that comes from adoption and the healing that can follow an abortion.
For us, every month is the month we witness, experience, and encounter these stories, so why even bother with Respect Life Month?
It's all about seasons. The seasons set aside in church life to celebrate such events as Easter and Christmas help fuel our appreciation and awareness about truths that should always be on our hearts and minds. We recognize the truth of Jesus rising from the dead every day, but that doesn't keep us from celebrating Easter. In the same way, we celebrate Respect Life Month to remind ourselves and others of the beauty and wonder of life from conception to natural death.
Reflect on this year's theme for a moment. "Each of us is a masterpiece of God's creation." When you go to an art museum and see a painting or sculpture worked by a master artist, what do you do?
Personally, I'm stopped in my tracks, breathlessly gazing on the beauty and wonder of the masterpiece. Between van Gogh's Starry Night, da Vinci's Mona Lisa, Rodin's The Thinker, and Rembrandt's The Return of the Prodigal Son - only a few of the recognized masterpieces of Western art - I could spend days in reflection and admiration.
And yet, these master artists are mere shadows and reflections of the Master Artist, whose masterpieces we so easily pass by without a second glance. God gives each of His masterpieces unique gifts of life, personality, and will. God's art is not stagnant or unthinking. Every person - each of us - is one of God's masterpieces.
When we take the time to gaze at His masterpieces, we can't help but notice the beauty and wonder of each man and woman, adult and child, pregnant mother and unborn baby.
This is the month to remind ourselves, our staff, our volunteers, our clients and our communities that each of us is a masterpiece. It's a time to remember that every life is worth celebrating, honoring, and cherishing as a precious and irreplaceable creation by the Designer and Maker of the universe.
Whether you have celebrated October as Respect Life Month with fundraising, awareness campaigns, or nothing at all, it's not too late to remind someone that they are a masterpiece. Those we serve certainly need this reminder, but so do our staff, volunteers, and everyone we see day by day.
Speaking of reminders, here is one for you: You are a masterpiece created by God, the Master Artist. Even if no one else does, He gazes on you with wonder, both in this season and in every season.
Strengthening the Core at Institute
by Jay Hobbs, Communications and Marketing Director
When leadership is discussed as a topic unto itself, most experts tend to zero in on models, theories, and examples.
How frequently should my team meet? How strictly should the Board abide by Robert's Rules of Order?
Should my title be Director? Executive Director? Grand Pooba?
As you may have guessed, the idea of sitting through an extended meeting to focus on these burning topics wasn't exactly on my Can't-Wait-To-Do List.
My fears were dispelled about 30 seconds into the Leadership track of this year's Heartbeat's Institute for Center Effectiveness.
Instead of wrangling about which leadership strategy has which benefits or holes in it, our facilitator, John Rue of Built to Lead, went straight to the heart when the starting gun fired.
John's point, from start to finish, was that, if we are ever going to lead—or even live—with freedom and conviction, the question of "Who" we are needs to be settled and fanned into flame.
Am I primarily a director? A leader? A pastor? A husband? A dad?
If so, I'm going to face an uphill climb any time any of those identities are threatened. Bad day at work? That's an assault on my primary identity as a director. Bad day at home? That's an assault on my primary identity as a husband and dad.
The biblical shorthand for all of this is idolatry. It's dethroning God and setting up something in His place. When we do that with our work, family, friends, or anything else, we're cutting ourselves off from our true identity: Believer, Son, Friend of God, Sheep. Not only that, but we're putting an astronomical burden on something (or someone) who was never intended to bear the weight of the universe.
That was the starting point for the week, where we focused on finding not "balance," but alignment between who we are and what we do. This is where our core identity aligns with our passion, and where work becomes a joyful outflow.
What's your primary identity? What are you passionate about? Do they line up? Maybe next year's Heartbeat's Institute for Center Effectiveness is a great place to find out.
Launching a Successful Year End Appeal
By Kirk Walden, Advancement Specialist
The Year End Appeal can be one of our most successful development initiatives of the year. This is our opportunity to tell our story, unveil new plans, and invite those who are in a giving frame of mind to join us in launching a successful 2015.
Ministries and organizations that forgo this opportunity miss out not only on gifts that can make a major difference in the bottom line, but also lose a great chance to begin building relationships with those who receive our other mailings.
There are reasons some ministries decide not to send a Year-End Appeal, but any objections to this endeavor are easily answered.
With mailing expenses, the Year-End Appeal costs too much
Let’s say we send 1000 letters, a $490 investment in postage. With envelopes, paper and ink, let’s say we spend as much as 50 cents per package on color printing. That’s about $1.00 per mailing. That’s $1,000. If ten out of 1,000 recipients send us $100, we’ve already broken even. A well-written year-end appeal will not lose money.
No one reads appeal letters
We can’t expect 50% response rates, because it is true that many people throw away appeal letters. Yet, every major non-profit sends appeal letters; they do so because they know this is a great way to reach new, and existing financial partners. In addition, many—especially the home-bound—only give to appeal letters.
We do appeal letters at other times of year. We do not want to overwhelm our donors with junk mail.
Take it from someone who signs up for newsletters from pregnancy help organizations all over: While you keep close track of your appeals, your recipients do not.
Occasionally someone will send a ministry a note saying, “You send too much mail,” but we absolutely cannot base our mailings on one or two complaints. People are busy—they don’t have time to worry about our number of mailings.
Most ministries do not send enough appeal letters. The Year End Appeal is at the top of the list. This month, let’s make it happen.